
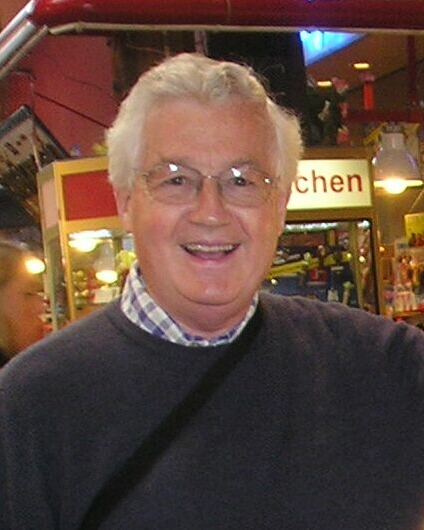
Roger's Story
 June 2005. I had known Roger for only four weeks when I was rung to be told that he had collapsed at home and been rushed to hospital. I found him in the Royal West Sussex Hospital in Brighton. (Why on earth have they decided to place the general hospital for the whole of West Sussex at the other end of a giant, permanent traffic jam?)
June 2005. I had known Roger for only four weeks when I was rung to be told that he had collapsed at home and been rushed to hospital. I found him in the Royal West Sussex Hospital in Brighton. (Why on earth have they decided to place the general hospital for the whole of West Sussex at the other end of a giant, permanent traffic jam?)
Roger was severely anaemic and the staff at the Digestive Diseases Department pumped him with antibiotics and gave him three endoscopies during the week he was there. Although I am sure the doctors did not see anything, they confidently declared it to be a duodenal ulcer and sent him home with another tablet for the morning medicine cabinet.
January 2006. Roger and I were heading for the Digestive Diseases Department to have an endoscopy. Roger had found a palpable lump in his abdomen and his GP sent him straight off for tests. The Royal West Sussex Hospital is built on the side of a cliff and whichever access you use involves climbing a steep incline, however unwell you feel. Roger complained that his legs were like lead and he could hardly lift them. Sure enough - severe anaemia - and he was kept in for tests. He was with a different specialist who suggested a CT scan as an afterthought (perhaps the lump was a bit of a giveaway), and there was the GIST, in the muscle tissue on the outside of Roger's stomach. No amount of endoscopies on the inside would have revealed it. He also had a small tumour above the primary GIST on his oesophagus. We christened them Gordon the GIST and Charlie the Chest. Naming them helped to reduce the fear of them.
Before Roger was discharged we saw a surgeon because he had had experience of GISTs. He told us that Gordon was so large that he could not operate to remove it because he would have to remove the whole stomach and that would kill Roger. He said it with such assurance we took his word for it. Glivec was described as a wonder drug that would reduce and remove the tumours without surgery. Sure enough, after a while the tumours changed their consistency and became soft like jelly.
Soon after Roger started on 400mg Glivec a day, he moved to Hampshire to be with me and he transferred to Southampton General Hospital. Several things were disconcerting, including the fact that we did not have a key worker assigned to ring up whenever we had questions or worries. The oncologist was quite reticent and did not tell us much after each CT scan. We felt very adrift and alone.
March 2007. The oncologist hinted that it might be possible to remove the tumour.
July 2007. Roger was very anaemic again and had to have a blood transfusion.
Aug 2007. The oncologist could not show us the latest CT scan because the computer was down. We were disappointed. He also discounted the idea of surgery. We joined the Gist Cancer Mailtalk at this point because we felt very uncertain about everything. This Mailtalk group made it very clear that we should get a second opinion and to go to a centre of excellence. Winchester is not far from London so we had a referral from Southampton to the Royal Marsden Hospital. After informing the Southampton oncologist that we would like a second opinion, he started to talk about surgery again and said he would arrange for a surgeon to see Roger.
September 2007. The oncologist showed us the scans at last. He said the tumour was getting bigger again, but he did not elaborate.
Later in September we went to the Royal Marsden Hospital to see Professor Ian Judson. He gave us a detailed description of what was going on - Gordon has developed a resistance to Glivec and shows evidence of blood vessels in places around its surface. Charlie is still responding to Glivec and shrinking. He said he would discuss Roger's case with his TEAM - a word we had not heard in any other hospital. In particular he wanted to talk to his surgeon, Mr Satvinder Mudan.
Two weeks later we saw Mr Mudan, who was very upbeat and said he thought surgery was possible and he wanted to get on with it and was setting up all the necessary pre-operation tests as we spoke. He suggested that it was unusual for a metastasis to grow above the primary tumour and in a later letter surmised that what Roger has is a dumbbell-shaped tumour and Charlie is an outcrop of Gordon.
Eighteen months after initial diagnosis, Roger is preparing for an operation which will include removal of his stomach, a procedure we had originally been told was not possible. Roger is now undergoing pre-op tests, heart tests (he has a history of heart disease) and finally he will have an endoscopic procedure under general anaesthetic before the big one. We received an appointment to see the surgeon in Southampton only after Roger was well into the tests at the Royal Marsden. Now that Gordon is growing again time is running out and we feel aggrieved that the regional hospitals did not refer Roger to the Royal Marsden Hospital for advice, since that is the place where the frontline research is being done. We now feel that at last Roger is being looked after by a team of doctors who really know about GIST.
Roger was keen to get Gordon and Charlie removed because he can feel that things are changing.
January 2008 dawned full of hope and apprehension. Roger was booked into the Royal Marsden for his attempted resection. The operation went ahead but in the end the tumour was not removed because Roger's blood pressure plummeted and it took an hour and a half to stabilise him again. This was near-death number one.
Roger spent the rest of February high on morphine. It was a leap year and I proposed to him. We were married in August 2008. It was a very joyous occasion followed by a cruise on the QE2. Soon after we came home he collapsed and was rushed to hospital with acute septicaemia. The Intensive Care consultant at The Royal Hampshire County Hospital in Winchester told us he would not survive and so four weeks after our wedding it looked as though I would be a widow. Roger had other plans and recovered. This was near-death number two.
In 2009 he became anaemic and was given more and more units of blood until he was receiving three units every week. One day he had a rant at his GP and told him to let him die or do something about the quality of his life. The GP considered things and referred Roger to a haematologist at RHCH. She put him on a course of daily injections of Epoetin Alfa (Eprex) which is designed to stimulate the bone marrow into producing blood cells. This had a dramatic effect on his health and even stopped the tumour from growing. This was near-death experience number three. Later it was shown that he had disease progression and was put onto Sutent. This lasted only six weeks as he could not tolerate the drug. One effect of the Sutent was that a big abscess developed under his operation scar and he had a big opening that oozed stomach fluids. We had to learn how to use stoma bags to deal with this which he then had for the rest of his life. He went back on to Glivec which seemed to start working again.
Most of 2010 was quiet. At the end of the year we spent Christmas in Edinburgh. The train journey home, however, was a nightmare and when we went back to A&E he was shown to be dangerously anaemic again. After he was stabilised at RHCH we went up to RMH in early 2011 for an experiment treatment firing targeted radiotherapy at the point in his stomach where the tumour was breaking through. It knocked him flat for about a month but then he was in rude good health again for quite some time. This was near-death number four.
In early 2013 Glivec was not working again and the RMH tried him on Regorafenib. Within a week he was completely wiped out and it took a month from stopping the drug for him to recover. After that he was taken off all inhibiting drugs as there were none that he could tolerate that would work. By Christmas 2013 he was getting slow and weak. The GP put him on a short dosage of steroids so that he could enjoy Christmas, which he did. In the middle of January 2014 he began to have internal bleeding and died on February 17th. From diagnosis in January 2006 Roger survived eight years with GIST. He saw his son marry and bestow two grandsons on him who were four and six when he died. He married me and stuck around to give me five and a half years of marriage. Most of all, despite some physical difficulties he had a tolerable normal life.
(Updated 15/10/2014)
>> Read More: GIST Patient Stories
